Program Evaluation Proposal For a Hospital Study Merle Canfield, PhD
This is a proposal is for a psychiatric hospital outcome study. It contains the study design, a set of proposed instruments, a schedule of data collection, an overview of statistical analyses, sample results of analyses, and cost of the project. The design has been used by program evaluators in a large private psychiatric hospital study (see Canfield, Muller, Clarkin, Whitmarsh & Thorward, 1988).
Six measures or scales are attached. The scales are selected to include outcome (pre- and post-measures of patient functioning), measure of treatment (the kind and amount of treatment received by the patient), previous history of the patient (previous illness, previous treatment, family information, etc.), and information about the interpersonal network of the patient.
The proposed measures are:
The Psychosocial Assessment Scale (Adult or Child)
The Psychotherapy Process Questionnaire
The Psychotherapy Session Questionnaire
The Setting Questionnaire
The Social Network Questionnaire
The Chart Review Form.
These scales cover the domains that we believe are necessary for an effective outcome study. We believe these scales are optimal for cost and effectiveness. However, we realize at some levels these are global measures and will not capture the totality of either treatment or outcome. Consequently, at the request of the hospital, either the domains or the scales may be revised. Other outcome measures that are popular are the BPRS and the SCL-90. Administration time and test cost should be considered when making substitutions. For example, one might consider using the MMPI for an outcome measure but the administration time would prohibit a telephone follow-up. Further, the cost of the test and scoring would be significant when one considers that the test may be administered to each patient a minimum of three times.
The Outcome Study Purpose
The objectives of the project are to:
Measure the effectiveness of treatment programs by assessing patient improvement.
Establish a relationship between treatment and outcome as moderated by patient status and environmental characteristics.
Develop models to predict optimal outcomes based on the influence and interaction of patient status and treatment elements.
The project enables the hospital staff to:
Use empirical models to develop effective treatment plans and to make daily treatment decisions. Maximize the probability of improved patient well-being in the most efficient manner.
Optimize the use of resources.
Demonstrate effectiveness to payers (optimal treatment may be longer for some patients).
Present results to the scientific community to contribute to the fund of knowledge and thus enhance hospital prestige.
Present results to the community served leading to informed choices, thereby, strengthening the hospital's reputation.
Summary of Variables, Method of Data Collection, Instruments Used in Data Collection
The following is a summary of categories to be assessed and the methods and instruments to be used in data collection. Table 1 outlines the (a) general information obtained, (b) time of collection, and (c) instruments used for data collection. Table 2 provides the specific variables to be measured.
Table 1. Data Collection Program.
![]()
![]()
Category Measured Time Instrument
![]()
Pre-admission Status | Admission | Chart Review Form; |
Demographics | Psychosocial | |
Prognostic Indicators | Assessment Scale | |
Patient Social Network | (Adult; Children) | |
Psychosocial Functioning |
Treatment Variables | During Treatment | Chart Review Form; |
and Diagnosis | Psychotherapy Session | |
Questionnaire; | ||
Psychotherapy Process | ||
Questionnaire; | ||
Setting Questionnaire | ||
Discharge Status Charts Reviewed Chart Review Form Following Treatment
Outcome--Patient Network, | Six Month and | Psychosocial | Assessment | |
Psychosocial Functioning | One Year Follow-up | Scale | (Adult; |
Children)
Social Network Questionnaire
![]()
![]()
Instruments
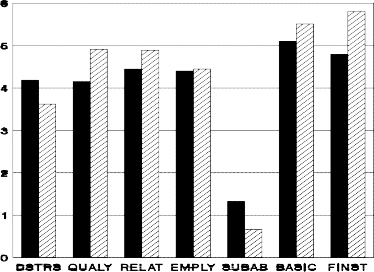
The Psychosocial Assessment Scale (PAS) is a 23 item inventory that utilizes a nine point (0 to 8) Likert-type scale. The patient rates each item according to the scale ranging from "none of the time" to "all of the time." Factor analysis of this measure yielded the following seven factors: Psychological Distress, Quality of Life, Relationships, Employment Functioning, Substance Abuse, Basic Living Skills, and Financial Stability.
The Setting Questionnaire (SQ) is a 27 item instrument that assesses the qualitative nature of the treatment setting based upon ratings by staff, patients and observers. The respondents rate the setting in terms of: conflict, cooperation, humor, tension, suspicion, independence, productivity, satisfaction, learning, coercion and enjoyment. The questionnaire assesses environments and identifies the characteristics that can, then, be related to patient outcome.
The Psychotherapy Session Questionnaire (PSQ) is a 20 item scale that measures the degree and type of psychotherapy that was administered during a psychotherapy session. The PSQ was developed to relate treatment to outcome.
As does the PSQ, the Psychotherapy Process Questionnaire (PPQ) is used to relate psychotherapy process to patient outcome. The PPQ is a 22 item instrument that the therapist completes by rating the degree to which he or she engaged in such therapeutic interventions and approaches as goal setting, confrontation, interpretation, reinforcement, emotional expression, homework, and so forth.
The Chart Review Form (CRF) was developed by the CNPHA collaborative research group (Canfield, Clarkin, Coyne and Grob, 1987). It provides information regarding the patient's previous hospitalizations and history of illness as well as information concerning treatment received during the current hospital episode.
The Social Network Questionnaire (SNQ) consists of 31 items that assess the patient's personal interactions and the types and quality of those interactions. The questionnaire measures a broad social network including mate, family, friends and co-workers. The Social Network Questionnaire may be completed by the patient or administered in a telephone interview (Canfield & Canfield, 1993).
Table 2 Specific Variables to Be Measured
----------------------------------------------------------------------------------------------------------------------------- -------------- PRE-ADMISSION STATUS
Demographics
Gender Marital Status
Prognostic Indicators
Impairment Index at Admission
Age at First Outpatient Treatment
Patient Network
Relationship with Mate
Psychosocial Functioning
State of Residence
Religion
Age at First Hospitalization
Age at First Treatment in Day Hospital
Relationship with Family
Primary Residence Prior to Admission
Total Days in Day Hospital
Number of Previous Hospitalizations
Relationships with Friends
Date of Birth
Years of Education
Total Number Days of Prior Hospitalizations
Family History
Relationships with Co-workers
Referral Source
Admission Status (e.g., Voluntary)
Admission Diagnosis Axes I and II
Living Conditions
Psychological Distress
Quality of Life Employment Functioning
Substance Abuse Basic Living
Skills
----------------------------------------------------------------------------------------------------------------------------- -------------- TREATMENT COMPONENTS
Length of Stay
Residential Placement
Therapist Physician
Number of Restraints
Number of Seclusions
Medication
Time Spent in Schooling
Chemical Dependence Program
Social Services Staff Involvement
Rehabilitation Program
Activity Therapy
Group Therapy
Family Therapy
Individual Therapy
Treatment Compliance
Patient's Perception of Therapy
Therapist's Perception of Therapy
----------------------------------------------------------------------------------------------------------------------------- -------------- DISCHARGE STATUS
Discharge Date
Nature of Discharge
Discharge Plan (Location)
Transfer Plan (Location)
Aftercare Plan
Discharge Diagnosis Axes I and II
Primary Diagnosis
----------------------------------------------------------------------------------------------------------------------------- -------------- FOLLOW-UP STATUS
Patient Network
Relationship with Mate
Psychosocial Functioning
Psychological Distress
Quality of Life Diagnosis
Employment Functioning
Relationships with Family
Substance Abuse
Relationships with Friends
Basic Living Skills
Financial Stability
Relationships with
Co-workers
Living Conditions
Data Collection Overview
Data are collected at the following intervals: Admission
During treatment Discharge
Six months after admission One year after admission
Data Collected at Admission
The following data categories are collected at admission: Pre-admission Status
Demographics Prognostic Indicators Patient Social Network Psychosocial Functioning
Selected variables from the measures of pre-admission status are repeated at the six month and one year follow-up intervals. Changes in pre-admission status are used to evaluate the treatment program. Pre-admission status information is acquired by hospital staff with the use of the Chart Review Form (CRF) and the Psychosocial Assessment Scale (PAS).
Data Collected During Treatment
Information regarding treatment variables and diagnoses is obtained during treatment. This information includes such data as:
Length of Stay Therapist
Therapy Modes Used Milieu Characteristics
Treatment data are collected by hospital staff with the use of the Chart Review Form (CRF), and the Setting Questionnaire (SQ).
PE Hospital Page5
Data Collected at Discharge
At discharge, information collected includes the following: Discharge Date and Plan
Discharge Diagnosis Primary Diagnosis
Patient's Perception of Therapy Therapist's Perception of Therapy
Discharge data are collected by hospital staff by using the following instruments: Chart Review Form (CRF), Psychotherapy Session Questionnaire (PSQ), and Psychotherapy Process Questionnaire (PPQ).
Data Collected at Follow-up
Five and one-half months and eleven and one-half months after admission, patients are mailed the Psychosocial Assessment Scale (PAS) and Social Network Questionnaire (SNQ). Approximately 40 percent of the mailed follow-up forms are typically returned by the patients. Two weeks beyond the initial mailing, patients who have not responded are contacted by telephone and reminded to complete and return the two forms. Four weeks beyond the initial mailing, the remaining patients who have not responded are contacted by telephone and forms are completed by the telephone interviewer. This interview takes approximately 20 minutes.
The follow-up data include such variables as: Relationships with Mate, Family, Friends and Co-workers Living Conditions
Psychological Distress Quality of Life Employment Functioning Substance Abuse
Basic Living Skills Treatment Status
Preliminary Report
The Preliminary Report generated by the Research, Evaluation & Statistics (RES) staff is prepared eight months after the project start date. It includes descriptive statistics regarding patient pre-admission status, general demographics, prognostic indicators, and psychosocial functioning. These data incorporate information obtained by the Psychosocial Assessment Scale and Setting Questionnaire. This report may be used as an initial feedback record of the project's process.
Interim Report
The Interim Report is prepared fourteen months beyond the project start date. This report relates pre-admission status to follow-up status. It includes data for patients who have been discharged and have participated in the six month data collection follow-up. Approximately 50 percent of the sample patient population will have completed the six month follow-up and will be included in the interim report. The report includes information obtained from each of the proposed measures (Psychosocial Assessment Scale, Psychotherapy Process Questionnaire, Psychotherapy Session Questionnaire, Setting Questionnaire, Social Network Questionnaire, and Chart Review Form).
Final Outcome Report
The Final Outcome Report is prepared twenty months after the onset of the project. It is a comprehensive integration of the broad categories measured (See Table 1) and the specific variables measured (See Table 2) by the six instruments. This report provides follow-up information for the total sample of patients who have completed the six month and one year follow-up. The Final Outcome Report includes information regarding:
The program's relationship to patient outcome, such as: Improved patient functioning
Improved social network Improved living conditions Improved quality of life
Improved employment functioning Decreased substance abuse Improved basic living skills
The relationship between modes of treatment and outcome
The relationships of patient chronicity and acuteness to treatment and outcome The relationships between diagnosis, treatment and outcome.
This report is designed to capture the complexity and interaction of patients, environments and treatments. Some patients need more treatment than others to make equal gains. Although this seems self- evident, it is not always taken into account by third party payers. This type of evaluation would give evidence by using the prognostic variables as mediators in the relationship between treatment and outcome. For example, two patients might enter the hospital with general feelings of worthlessness. The acute patient might gain a sense of worth with one week of treatment while the chronic patient might gain a sense of worth with one month of treatment. These differential effects of treatment are taken into account in this design. The prognostic variables will be used to moderate the effect of treatment on outcome to provide a more accurate picture of the relationship.
Further questions to be answered by the analysis include: What is the comparative impact of individual therapy, group therapy, and medications? What is the comparative impact of the directive approaches and cognitive approaches? What are the differential effects of these two approaches on different patients? The directive approach might benefit one type of patient and be detrimental to another type of patient. The approach of the design is to test these differential effects.
Sample Report Excerpts
The following samples illustrate samples of the various analyses to be performed by CSPP. Any of the variables in the system may be related to any other variable in the system. CSPP researchers may test many relationships as hypothesized in the literature (Canfield, et. al., 1988). The hospital will also specify a number of relationships to be tested.
Sample 1
Figure 1 displays the means obtained from patients at admission and at six months on each of the seven PAS subtests. This example shows that on the average, patients improved in all areas measured by the Psychological Assessment Scale. It should be noted that for the Psychological Distress (DSTRS) and Substance Abuse (SUBAB) variables, the desired direction is a decrease. T-tests conducted on each pair of means demonstrate, with the exception of Employment Functioning, that the six month follow-up ratings are consistently (and statistically significantly) better than the ratings upon admission. These results suggest that the hospital treatment is beneficial to patients by reducing their psychological distress and substance abuse, and improving their quality of life, relationships, basic skills and financial stability.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Figure 1. With the exception of employment, the admission score, in each case, is significantly different than the six month score.
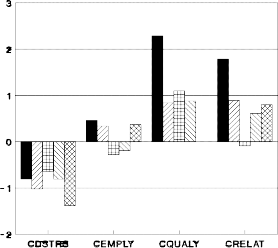
Figure 2 displays change scores between admission and the six month follow-up obtained from patients with different diagnoses. Affective, Anxiety, Borderline Personality Disorder, other Personality Disorders and Psychotic diagnoses are differentiated in their change scores on the Psychological Distress, Employment Functioning, Quality of Life and Relationship subtests. Psychological distress was decreased for all five diagnostic groups with patients diagnosed Psychotic showing the greatest reduction in perceived distress. Both Quality of Life and Relationships were generally improved, with patients suffering from affective disorders indicating the greatest changes. Interestingly, patients diagnosed Borderline showed no change in relationship functioning, and those diagnosed Psychotic showed no change in their Quality of Life from admission to follow-up.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Figure 2. Change scores of the Psychosocial Assessment Scale plotted by diagnosis.
Figure 3 represents change scores by number of previous hospital admissions. Treatment affects psychological distress, employment, quality of life and relationship factors differentially based on the chronicity of the patient. The number of previous hospitalizations was used as an indicator of chronicity experienced by patients. While all patients, regardless of previous number of admissions, tended to report an improvement in their quality of life, first time admission patients showed the most significant reduction in psychological distress from admission to follow-up. Patients with four or more prior admissions also showed a slight decrement in employment functioning following treatment, whereas, first, second and third time admission patients tended to improve in this area. On the Relationship subtest, all patients, except the most chronic (with five or more previous admissions), improved.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
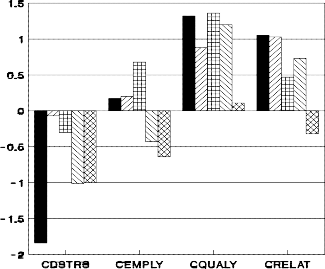
Figure 3. Change scores on the Psychosocial Assessment Scale plotted by number of previous admissions.
Sample 4
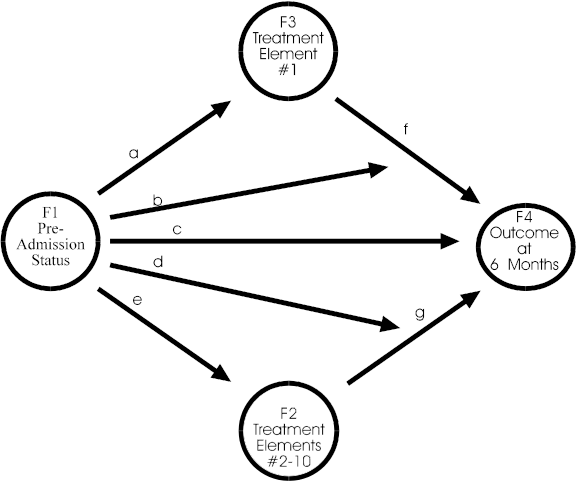
A major thrust of this design is to determine what elements of the treatment affect what elements of outcome for what type of patient. All of these elements--treatment, outcome and patient status--need to be measured. Historically, status and outcome have been extensively measured. Whereas, treatment has not been measured to this extent. Consequently, a primary objective of this design is to include treatment measures within the process. The diagram in Figure 4 is used as a guide for this section.
Two concepts are important in assessing the effects of treatment on different types of patients. These concepts are: (a) mediation, and (b) interaction. Mediation is the effect of treatment or some other influence on the pre-admission status. If it were not for this mediation, it would be assumed that the status of the patient would not change so that at the six month follow-up the patient would be the same as at admission. For example, the score on Psychological Distress at admission (F1--pre-admission status) should be a predictor of Psychological Distress at six months follow-up (F4--outcome at six months). However, the six month score will be changed or "mediated" by treatment (F3--treatment element #1 and F2--treatment elements #2-10). The relative strength of these two mediating factors can be tested for their impact on outcome. Interaction occurs when patients differ in response to treatment. Some patients will be influenced by one treatment while other patients may not be influenced by the same treatment.
The analyses test mediation and interaction. Consequently, the results will take the form of "block diagrams" representing these two concepts as illustrated in Figure 4. The circles represent factors of either status, treatment or outcome, and the arrows represent the direction of influence and interaction. When an arrow leads from one circle to another circle it represents the influence of one factor on another. When the arrow points to another arrow (e.g., "b" to "f"), it represents an interaction of the three factors connected by the arrows (e.g., F1, F3, and F4 in Figure 4). An example would be if Patient A (diagnosis phobic) were influenced by Treatment X, and Patient B (diagnosis schizophrenic) was not influenced by Treatment X.
Figure 4 shows a model to be tested. Each of the arrows (a through g) can be tested for the impact they represent. They can be tested individually or as part of the full model. For example, if all arrows but "c" were removed and "c" were found to be significant, one might conclude that the pre-admission status determines the outcome. That is, diagnosis, severity, degree of distress, etc. (F1--pre-admission status), predict outcome at six months (F4). However, if Treatment Element 1 (F3) is included (suppose that were individual therapy) then the significance of "c" is decreased or even reduced to 0. Further, Treatment Elements 2 though 10 (F2) could be added to assess the impact of Treatment Element 1. The arrows "b" and "d" represent interactions between patient status, treatment and outcome.
This example has represented one possible model to be tested. As there will be at least 65 variables assessed in the proposed study (see Table 2), there are, theoretically, over 2000 models that could be tested. The RES staff will test a number of models (see Canfield, et. al., 1988). The hospital staff is expected to generate a number of models based on their expectations and experience. RES will test 15 hospital generated models.
![]()
RES Project Timetable
Table 3 outlines the time line for data collection and the preliminary, interim and final reports.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Implementation
Once the hospital decides to implement the project, it takes approximately 4 months to begin data collection. The actual amount of preparation time depends primarily on the hospital. Time must be allotted to inform the staff, solicit their participation, set up the system, train personnel, conduct a review process, and so forth.
Although instruments have been proposed, the clinical staff may have suggestions for other instruments or other methods of gathering the same data. CSPP will work with the staff in the use and/or development of different instruments. If this process becomes extensive, it could further delay the start of data collection.
On Site Data Collection
Four of the questionnaires are completed at the hospital site, consequently, the hospital staff performs these tasks. Two of the questionnaires, the Psychosocial Assessment Scale (PAS) and the Social Network Questionnaire (SNQ), are administered immediately following admission (within 24 hours or within 48 hours at the most). Admission staff or ward personnel have been found to be the most effective administrators of the questionnaires. However, both of these groups probably have full schedules and it may be desirable to hire a person for the purpose of administering these questionnaires. The patients will usually complete the two questionnaires without assistance in about 15 minutes. In such cases, the staff time involves handing the questionnaires to the patient and retrieving them. On some occasions, the patient may be unable to complete the questionnaires (e.g., young children and non-readers), therefore, the person administering the questionnaires will need to interview the patient.
The two questionnaires that are administered at discharge (PPQ and PSQ) are very similar to the admission
questionnaires in terms of time and effort required. The administration of the questionnaire to the patient, again, must be timely in that it must be done before the patient leaves the institution. The questionnaire that the primary therapist (Psychotherapy Process Questionnaire) completes is not as critical in terms of time. Ideally, the therapist should complete PPQ at the time of discharge. If patients are readmitted, they do not restart the process. They, instead, complete the 6 month and 12 month administrations on their prior schedules.
It is crucial that a designated person monitors the questionnaire administration process. If the questionnaires are not being completed, a monitor needs to be aware so that corrective action may be taken. If questionnaires are not collected on schedule, there is no time for "catching up"; they are simply missed and not part of the study. It is, therefore, recommended that the questionnaires be forwarded to RES as they are collected to provide a second monitoring process.
The Setting Questionnaire (SQ) is completed monthly by all staff and patients on the unit at the appointed time of administration. The SQ is administered for the day, evening and weekend shifts. If the weekend shift is not different from the day and evening shifts, then the SQ does not need to be administered a second time. Although the questionnaire typically takes about 10 to 15 minutes to complete, it will probably take about an hour for the test administrator to complete the total process.
The chart review is approximately a 2 hour process. Charts are reviewed for those patients who have completed all of the other questionnaires, including the 6 month follow-up questionnaires. The chart reviews are performed at the 12 month and 18 month phases of the project.
The 6 month follow-up questionnaires are administered to the patient in the following manner. Five and one-half months from the time of admission (note that this is not five and one-half months from the discharge of the patient), the patient is sent the PAS and SNQ with a request to complete the questionnaires and return them by mail. If the patient does not return the questionnaires, then a research assistant telephones and asks the patient if he or she has received the questionnaires and whether they have been completed. Frequently, the patient will complete the questionnaires at that time and return them. If the patient does not return the questionnaires after the first call, he or she is called again and interviewed by telephone with the research assistant completing the questionnaires. It should be noted that the letters sent to patients include a return card on which patients can indicate that they wish to be contacted by phone. This process takes about one hour for each patient contacted.
A 1/4 or 1/2 FTE is needed to accomplish all of the on-site tasks of this project. If the same person also performs the chart reviews, follow-up, and data entry, the time allocation may increase to about 1/2 to 3/4 FTE. Time allocation also depends on the number of patients being admitted and discharged. The workload will increase as the project progresses.
The two basic plans are as follows: Plan I
Plan I specifies that the hospital gathers the data in consultation with CSPP. The CSPP researchers design the project, sets up the computer systems, trains project participants, performs the analysis, and writes the report. If this plan is adopted, the hospital is responsible for supervising and maintaining the integrity of the data. A hospital staff member performs the duties of Principal Investigator.
Plan II
Plan II stipulates that the hospital gathers the data needed daily, weekly, and monthly on site (i.e., admission Psychosocial Assessment Scale, Psychotherapy Process Questionnaire, Psychotherapy Session Questionnaire, and Setting Questionnaire). The plan specifies that CSPP collects the follow-up questionnaires (Psychosocial Assessment Scale and Social Network Questionnaire at 6 months and 1 year). According to this plan, CSPP designs the system, sets up the computer system, trains project participants, enters the data, provides quality control, performs the analysis, and writes the report. Plan II states that the CSPP staff performs the duties of Principal Investigator.
Once the data are entered and analyzed, they are available to the hospital in dBase IV format with documentation so that the hospital could perform further analyses. Similar hospitals may want to perform comparison analysis, however, this is not recommended since various hospitals may have considerably different clientele that would affect the outcome.
ATTACHMENTS
PAS Psychosocial Assessment Scale (Adult or Child) PPQ Psychotherapy Process Questionnaire
PSQ Psychotherapy Session Questionnaire SQ Setting Questionnaire
SNQ Social Network Questionnaire CRF Chart Review Form
References
Canfield, M. L., Muller, J., Clarkin, J., Whitmarsh, J., Thorward, S. J., & Embretson, S. (1988). Issues in research design in psychiatric hospitals. The Psychiatric Hospital, 19, 11-26.
Canfield, M. L. & Canfield, J. E. (1993). A Collection of Psychological Scales. Bartlesville, OK: Coder Press. Canfield, M. L., Clarkin, J., Coyne, L., & Grob, M. (1987). Reliability of data taken from medical charts. The
Psychiatric Hospital, 17, 173-179.
Psychosocial Assessment Scale
Name:_
ID #
Date
Circle the number below that is the closest to how you have felt recently.
none all
IN THE PAST WEEK HOW OFTEN HAVE YOU ... of the several of the
1. | ...enjoyed your leisure hours (evenings, weekends, etc.)? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
2. | ...felt fearful or afraid? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
3. | ...felt sad or depressed? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
4. | ...felt good about yourself or things you have done? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
5. | ...felt angry? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
6. | ...felt mixed up or confused? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
7. | ...felt like you've spent a worthwhile day? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
8. | ...felt tense? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
9. | ...felt useless? | 0 | 1 | 2 3 | 4 | 5 | 6 | 7 | 8 | ||||
very | very | ||||||||||||
time times time
IN THE PAST WEEK ...
dissatisfied satisfied
...how satisfied have you been in general (with relationships, with finances, 0 1 2 3 4 5 6 7 8
and family?)
never often
...how often did you get together with people outside of your home? 0 1 2 3 4 5 6 7 8
all of
never the time
...did you handle the basic necessities such as paying bills, shopping and 0 1 2 3 4 5 6 7 8
and taking care of your room (home; apt.)?
none some much
...how much time did you spend with friends & family talking or doing things 0 1 2 3 4 5 6 7 8
together?
a great
none some deal
...how much conflict was there with the person(s) you live with? 0 1 2 3 4 5 6 7 8
...have you used alcohol? 0 1 2 3 4 5 6 7
8
...have you used drugs? 0 1 2 3 4 5
6 7 8
--------------------
How much would friends or community members support you if you were sick 0 1 2 3 4 5 6 7 8
or having problems?
part full
not
employed time time
Are you employed (includes self-employed, housewife, student, employee)? 0 1 2 3 4 5 6 7 8
19. Do you feel that you do a good job (whether self-employed, housewife, 8 | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
student, employee)? | ||||||||
8 | 0 0 | 1 1 | 2 2 | 3 3 | 4 4 | 5 5 | 6 6 | 7 7 |
8 |
not at all completely
no enough
22. In the past month, was the amount of money you had, enough to pay the bills? 0 1 2 3 4 5 6 7 8
poor | good | |
23. Do you feel that you are in good physical condition? | 0 1 | 2 3 4 5 6 7 |
8 | ||
5-6-93 |
Psychosocial Assessment Scale (Children)
Name:_
ID #
Date
none | all | ||
IN THE PAST WEEK HOW OFTEN HAVE YOU ... | of the | several | of the |
time | times | time |
Circle the number below that is the closest to how you have felt recently.
1. | ...had a good time playing? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
2. | ...felt fearful or afraid? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
3. | ...felt sad or depressed? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
4. | ...felt good about yourself or things you have done? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
5. | ...felt angry? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
6. | ...felt mixed up or confused? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
7. | ...felt like you've spent a worthwhile day? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
8. | ...felt tense? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
9. | ...felt useless? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
not | |||||||||||||||
IN | THE PAST WEEK ... | liked |
liked
...have you liked the way things have gone (with your friends, with your family 0 1 2 3 4 5 6 7 8
have things you need?)
never often
...how often did you go outside or to friends' houses to play? 0 1 2 3 4 5 6 7 8
all of
never the time
...did you do your chores (like cleaning your room, helping your parents, 0 1 2 3 4 5 6 7 8
keeping yourself neat and clean)?
none some much
...how much time did you spend with friends & family talking or doing things 0 1 2 3 4 5 6 7 8
together?
never some usually
...have you been getting along with people who live in your house? 0 1 2 3 4 5 6 7 8
a great
never some deal
...have you used alcohol? 0 1 2 3 4 5 6 7
8
...have you used drugs? 0 1 2 3 4 5
6 7 8
--------------------
How much would friends or community members support you if you were sick 0 1 2 3 4 5 6 7 8
or having problems?
some of
no the time yes
18. Do you go to school (when school is open)? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
8 | ||||||||
19. Do you feel that you do a good job at school? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
8 | ||||||||
20. Do you like school? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
8 | ||||||||
21. Do your feelings and thoughts keep you from doing your school work? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
8 |
Are you healthy? 0 1 2 3 4 5 6 7
8
5-6-93
Number of sessions completed:
Gender:
Date:_
Use the scale below to rate your MOST RECENT PSYCHOTHERAPY session.
Strongly Strongly
Disagree Disagree Neutral Agree Agree
0 1 2 3 4 5
6 7 8
Circle the number that best represents your attitude.
IN THE PSYCHOTHERAPY SESSION THE THERAPIST...
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | was interested in me. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | accepted our differences. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | knew what I was talking about. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | was comfortable. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | was clear. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | listened to me. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | talked a lot. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | made specific suggestions. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | was on the same track with me. |
IN THE PSYCHOTHERAPY SESSION I...
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | felt hopeful. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | made a plan to deal with my problem(s). |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | felt better. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | saw my problems as solvable. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | moved toward my treatment goal(s). |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | recognized things that I didn't know about before. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | felt involved. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | saw things in new ways. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | talked about my past. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | talked about my relationships. |
0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | benefitted from therapy. |
Name:
Patient:
Use the scale below to rate the way you usually respond in psychotherapy.
none of a little of some of a lot of all of
the time | the time | the time | the |
time | the time |
0 1 2 3 4 5
6 7 8
IN PSYCHOTHERAPY SESSIONS WITH THE ABOVE PATIENT I:
0 1 2 3 4 5 6 7 8 helped the patient to identify specific goals of treatment.
0 1 2 3 4 5 6 7 8 worked toward specific goals.
0 1 2 3 4 5 6 7 8 intervened with family on behalf of the patient.
0 1 2 3 4 5 6 7 8 intervened with staff on behalf of the patient.
0 1 2 3 4 5 6 7 8 confronted the patient.
0 1 2 3 4 5 6 7 8 let the patient choose topics to talk about.
0 1 2 3 4 5 6 7 8 identified internal conflicts.
0 1 2 3 4 5 6 7 8 allowed tension to build between the patient and myself.
0 1 2 3 4 5 6 7 8 interpreted the patients thoughts and behavior.
0 1 2 3 4 5 6 7 8 allowed the patient to behave in a ways that I personally disagreed with.
0 1 2 3 4 5 6 7 8 gave "homework" to the patient.
0 1 2 3 4 5 6 7 8 had a plan of reinforcing the patient for positive behavior.
0 1 2 3 4 5 6 7 8 expressed disagreement with the patient.
0 1 2 3 4 5 6 7 8 talked about the "here and now".
0 1 2 3 4 5 6 7 8 asked questions about the patient's early development.
0 1 2 3 4 5 6 7 8 emphasized relationships.
0 1 2 3 4 5 6 7 8 talked.
0 1 2 3 4 5 6 7 8 felt close to the patient.
0 1 2 3 4 5 6 7 8 felt distant from the patient.
0 1 2 3 4 5 6 7 8 encouraged the patient to make his/her own choices.
0 1 2 3 4 5 6 7 8 set limits.
0 1 2 3 4 5 6 7 8 encouraged the patient to express repressed emotions.
SETTING QUESTIONNAIRE
NAME
DATE
SETTING
TIME
INSTRUCTIONS: For each item draw a circle around the number that you think best describes the setting according to the following scale.
│ | none of | a little of | some of | a lot of | all of │ |
│ | the time | the time | the time | the time | the time │ |
┌────────────────────────────────────────────────────────────────────┐
├────────────────────────────────────────────────────────────────────┤
│ 0 1 2 3 4 5 6 7 8 │
└────────────────────────────────────────────────────────────────────┘
IMPORTANT: If you think that some people are acting or feeling one way and other people are acting or feeling another way then both may be circled. Two numbers may be circled for one item. Do not circle more than two. Try hard to circle only one.
When people are in this setting they are:
1. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | tense |
2. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | satisfied |
3. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | easy going |
4. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | caring |
5. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | good |
6. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | friendly |
7. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | confident |
8. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | suspicious |
9. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | lazy |
10. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | forced to do things |
11. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | busy |
12. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ordered around |
When people are in this setting they:
13. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | have a say about what to do |
14. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | share |
15. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | know what's going on |
16. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | think |
17. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | work together |
18. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | have high self-esteem |
19. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | learn |
20. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | joke around |
21. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | can come and go as they want |
22. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | talk about personal problems |
23. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | have a good time |
In this setting:
24. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | things get done |
25. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | its easy to fit in |
26. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | there is conflict |
27. | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | people like each other |
1-14-91
Social Network Questionnaire
Name:
Age:
Gender:
For items numbered 1 through 24 consider the following people: spouse or mate, family, friends, people at work/school, or acquaintances. Leave the item blank if it does not apply to you. For example, if you are not married or living with someone, items 1 through 6 would be left blank. Think about each of those persons listed and the kind of activity you had with them. You should have an entry for each item according to the following:
8 = daily
7 = five or six times per week 6 = two to four time per week
5 = about once a week
4 = two or three times per month 3 = about once a month
2 = two to eleven times per year 1 = about once a year
0 = never
feel | get | share in | share in | |||
talk | conflict | close | support | productive | leisure | |
with | with | to | from | activity | activity | |
spouse or mate | 1. | 2. | 3. | 4. | 5. | 6. |
family | 7. | 8. | 9. | 10. | 11. | 12. |
friends/acquaintances* | 13. | 14. | 15. | 16. | 17. | 18. |
people at work/school | 19. | 20. | 21. | 22. | 23. | 24. |
* NOTE: If some people are both co-workers (or classmates) and friends, then rate the time
spent with them outside of work (school) as friends and the time at work (school) as co-workers (or classmates).
My living condition is: (check one)
( ) Live with family
( ) Live alone
( ) Live with relative(s)
( ) Live in psychiatric institution
( ) Live in halfway house
( ) Live with someone other than relative
( ) Live in foster home
CHART REVIEW FORM
Last Name_
First Name_
Middle
Med Rec #
Admit Date_
Discharge Date
Hospital
Address
City/State/Zip
Date of Birth Phone No.
Marital Status:
Never married
Married
Separated
Divorced
Widowed
(9) Unknown
Gender: (M) Male
(F) Female
Age:
Race: (1) Caucasian
African-American
Hispanic
Asian
Native American
Other
Unknown
Religion:
None
Catholic
Jewish
Protestant
Other
Unknown
Years of Education:
![]()
Highest Degrees Obtained:
Occupation:
Primary Therapist: Admitting
Physician: Service Code: Unit Code:
Total Days in Hospital Unit or Outpatient Programs:
Inpatient Hospitalization
Adult Open
PICU
Youth Serv.
Detox.
Rehab.
Partial Hospitalization
Adult
Adolescent
Child
Attending
Physician:
Referral Source:
Self
Family/Friend
Transfer From Other Inpatient
Psychiatrist
Physician Other than Psychiatrist
Court/Police
Psychologist
Other Mental Health Professional (LCSW,MFCC)
Unknown
Other
Nature of Current Admission:
Voluntary
Involuntary
Unknown
Primary Residence During Last 3 Months Prior to This Current Hospitalization:
Living with parents/grandparents
Living with spouse/significant other and/or child.
Alone
Halfway house
Group house/sheltered housing
Prison/juvenile detention center
School/dormitory housing
Foster parents
Missing
Residential treatment facility
Transfer from other institution
Other Include transfers from other institutions
Age at First Outpatient Treatment_
Psychiatric
Chemical Dependency
Emotional Problems
Age at First Hospitalization for Mental Illness (may be in a general medical
hospital)
Please enter patient's age when:
Adopted by nonbiological parents Adopted by
stepfather Adopted by
stepmother
Mother
died Adoptive mother
died Stepmother
died
Father
died Adoptive father
died Stepfather
died
Divorce between biological parents Divorce between adoptive parents
Divorce between one biological parent and a
stepparent_
Number of Previous Hospitalizations for Mental Illness
Total Number of Days Hospitalized for Mental Illness
Prior to this Admission
History of Mental Illness, Suicide or Alcoholism:
Mother | Father | Sibling | Grandparent | Children | Other Relatives | |||
y | y | y | y | y | y | |||
n | n | n | n | n | n | |||
u u u u u u | ||||||||
y = yes n = no u = unknown | ||||||||
Impairment Index at time of Admission: | ||||||||
Reality Orientation | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Danger to Self | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Danger to Others | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Danger to Property | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Following Prescribed Treatment Regimen | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Activities of Daily Living | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Role Performance | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Intimate Relationships | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Admission diagnosis: Axis I | ||||||||
![]()
![]()
![]()
Admission diagnosis: Axis II
![]()
![]()
Axis III:
Physical disorders and conditions
![]()
![]()
Axis IV:
Severity of stressor:
(1) None | (4) Severe | (9) Inadequate information |
(2) Mild | (5) Extreme | |
(3) Moderate | (6) Catastrophic |
Predominant type of stressor
Axis V:
Current GAF_
(1) 90-81 | (4) 60-51 | (7) 30-21 | (10) 10-1 |
(2) 80-71 | (5) 50-41 | (8) 20-11 | |
(3) 70-61 | (6) 40-31 | (9) Inadequate information |
Highest GAF in the past year
Number of:
Restraints Seclusions ECT Suicide Attempt
Number of:
AWOL times days LOA_
Please estimate the number of hours of treatment for each of the following categories:
SCHOOLING: Time spent in school program
CHEMICAL DEPENDENCY: Evaluation or participation in either individual or group or individual sessions
SOCIAL SERVICES: Family or Individual Casework.
Professional staff time spent with individuals or
their families. Include discharge planning
REHABILITATION: Individual or group work includes assertiveness training and work rehabilitation
ACTIVITY THERAPY: Time spent in all activities
includes music therapy, art therapy and so forth
GROUP THERAPY: Formal group therapy. Regular
meetings with professional staff
INDIVIDUAL THERAPY:_
Compliance with treatment:
Refused Treatment (1)
(2) Resistant (3)
(4) Compliant (5)
(6) Participative (7)
Active Engagement
Unknown
(1) | None | |
(2) | Anxiolytic |
|
(3) | Antidepressant |
|
(4) | Antipsychotic |
|
(5) | Lithium |
|
(6) | Anti-Parkinsonian |
|
(7) | Hypnotics |
|
(8) | Stimulants |
|
(9) | Anticonvulsants |
|
Psychotropic Medications Received During Hospitalization: Type of Medication Length of time on Meds
![]()
Other
Nature of Discharge:
Planned discharge
Discharged AMA
Time-limited for financial reasons
Time-limited by outside utilization review group
Elected by patient/family for other than financial reasons
Hospitalization stay extended while waiting for appropriate placement in another facility
Elected by staff for other than therapeutic goals or financial reasons
Patient deceased
Discharged for medical (physical illness) reasons
Other
Patient was discharged to the following residence:
Living with parents/grandparents
Living with spouse/significant other and/or child
Alone
Halfway house
Group house/sheltered housing
Prison/juvenile detention center
School/dormitory housing
Foster parents
Missing
Residential treatment facility
Other
Transferred to Another Institution: (circle one)
Acute General Hospital
Nursing Home/Extended Care Facility
Private Psychiatric Hospital
State Psychiatric Hospital
Veterans Hospital
Not applicable
Evidence of Formal Discharge Planning or Ongoing Aftercare Plans:
Outpatient Care
Residential Treatment
Partial Care
Private Practitioner Office Visits
Psychotropic Medication Therapy
Case Management by This Hospital
Managed Care by Outside Company
Other
Discharge Diagnosis:
![]()
![]()
![]()
![]()
Axis I: Axis II:
![]()